 A new review article on Vitamin by Dr. Michael F. Holick and Dr. Arash Hossein-Nezhad appears to confirm mounting evidence regarding the many health benefits of Vitamin D. Their article is “Vitamin D for Health: A Global Perspective.” It was published in the July 2013 issue of Mayo Clinic Proceedings.
A new review article on Vitamin by Dr. Michael F. Holick and Dr. Arash Hossein-Nezhad appears to confirm mounting evidence regarding the many health benefits of Vitamin D. Their article is “Vitamin D for Health: A Global Perspective.” It was published in the July 2013 issue of Mayo Clinic Proceedings.
You may wish to view the entire article (click here for the full text of the article (.pdf format), as I will only present selected findings because the scope of their article is beyond what I can readily summarize.
We at HPDI recommend high dose Vitamin D supplements (up to 5,000 IU daily for adults), like our Vitamin D3 Plus formula, especially in winter and northern latitudes, where no amount of winter sunlight can generate adequate vitamin D levels in the body.
Ever more evidence continues accruing about the importance of Vitamin D, its health benefits when optimal amounts are made available to the body, and the detriments to health when the body fails to receive adequate amounts (or when a state of deficiency occurs).
Because the preponderance of scientific evidence overwhelmingly supports the need for higher Vitamin D intakes, I feel it is important to highlight some of the authors’ findings in this study.
MAIN POINTS OF THE NEW VITAMIN D STUDY
Drs. Holick and Hossein-Nezhad emphasize several points:
1) Vitamin D deficiency is common and underdiagnosed.
2) An effective strategy to prevent Vitamin D deficiency and insufficiency is to obtain some sensible sun exposure, ingest foods that contain Vitamin D, and take a Vitamin D supplement.
3) Evidence from hundreds of recent studies suggests that Vitamin D is important for reducing the risk of type 1 diabetes mellitus, cardiovascular disease, certain cancers, cognitive decline, depression, pregnancy complications, autoimmunity, allergy, and frailty.
4) Vitamin D deficiency during pregnancy may influence fetal “imprinting” that may affect chronic disease susceptibility shortly after birth, as well as later in life.
5) The blood level of 25(OH)D is the best method to determine Vitamin D status.
DEFINING SUFFICIENCY AND DEFICIENCY OF VITAMIN D3
The authors note that the US Endocrine Society recommends that serum 25(OH)D levels of 30 ng/mL be attained to avoid risks connected with an inadequate Vitamin D status.
The Endocrine Society consequently recommends Vitamin D deficiency be defined as a 25(OH)D level of 20 ng/mL or less, vitamin D insufficiency as 21 to 29 ng/mL, and vitamin D sufficiency as 30 ng/mL or greater for children and adults. It suggested that maintenance of a 25(OH)D level of 40 to 60 ng/mL is ideal, and that up to 100 ng/mL is safe.
Maintenance levels can easily be attained in adults by taking 5,000 IU daily. Children can achieve maintenance levels when taking much less, e.g., 400–1,000 IU daily.
SELECTED FINDINGS
WHO IS DEFICIENT IN VITAMIN D3?
20%–80% of US, Canadian, and European adults (men and women) are deficient in vitamin D. Serum 25(OH)D levels less than 20 ng/mL was almost one-third of the US population (32%). More than 70% of non-Hispanic African-American individuals and more than 40% of Mexican-American Hispanic individuals were at risk for a 25(OH)D level less than 20 ng/mL (742).
Among Canadians, serum 25(OH)D levels less than 30 ng/mL were evident in 57.5% of men and in 60.7% of women, rising to 73.5% in spring (among men) and 77.5% in winter (among women) (742). Vitamin D deficiencies are high among populations in Europe, the Middle East, Asia, and many other areas of the world.
In contrast, high circulating vitamin D levels are found among individuals from tribal groups in east Africa. Individuals from these tribes receive tropical sunlight on their skin daily and exhibit a mean circulating 25(OH)D level of 46 ng/mL (743).
Darker skinned people, of course, have natural sunscreen protection due to their increased melanin skin pigmentation. Consequently, they are 90% less efficient in producing vitamin D in their skin compared with light-skinned individuals. Dark skinned people living in northern latitudes, for example, exhibit far greater incidence of vitamin D deficiency.
Individuals with dark skin living in the north, must therefore be diligent with respect to obtaining sufficient vitamin D from a combination of sun exposure, diet, and vitamin D supplements.
SUNSCREENS AND AIR POLLUTION
The prevalent use of sunscreens also contributes to vitamin D deficiency. For example, the authors note that a sunscreen with a sun protection factor (SPF) of 30 applied properly can reduce the skin’s ability to produce vitamin D by 95%–99% (743).
An often neglected factor in vitamin D deficiency is air pollution. Increased ozone and nitrogen dioxide levels (known to compromise several health outcomes) absorbs UV-B radiation. Individuals living in urban areas or other centers with high levels of air pollution are therefore also at higher risk for vitamin D deficiency.
Indoor living must be included on the list of lifestyle factors that cause vitamin D deficiency. Individuals living sedentary lives, mostly indoors and who avoid sun exposure (perhaps because they have been told to stay out of the sun) exhibit lower levels of vitamin D. As an example, institutionalized individuals constitute a well known risk group for deficiency (742).
MUSCULOSKELETAL CONSEQUENCES OF DEFICIENCY
The study authors find that current evidence from biochemical testing, observational studies, and randomized controlled trials suggest that serum 25(OH)D levels of at least 20 ng/mL are necessary for optimal bone and muscle function (with many experts regarding 30 ng/mL as the threshold for optimal bone health) and to minimize the risk of osteomalacia.
The study lists skeletal consequences of 25(OH)D insufficiency as including secondary hyperparathyroidism, increased bone turnover and bone loss, and increased risk of low-trauma fractures (727).
NON-SKELETAL HEALTH BENEFITS OF VITAMIN D
The authors note that studies show decreased risk of many disorders, including certain types of cancer, mental disorders, infectious disease, cardiovascular disease, type 2 diabetes, as well as autoimmune disorders, associated with serum 25(OH)D levels greater than 28 to 32 ng/mL. They point out that it has been argued therefore that 25(OH)D levels should be in the range of 28–40 ng/mL to maximize nonskeletal benefits.
The authors also report vitamin D deficiency is associated with an increased risk of total mortality (735).
Receiving adequate maintenance levels of vitamin D is not difficult, especially when vitamin D3 supplements are readily available, and the fact the sunshine is abundant, at least during the summer months in most locations.
Given the vast health benefits of vitamin D intake, there is every reason for individuals to ensure that they get adequate levels, and therefore at least avoid deficiency. Ideally, everyone should strive for optimal amounts that help create and maintain good health.
EPIGENETICS
The authors report that evidence from hundreds of studies suggests that vitamin D is important for reducing the risk of a variety of chronic illnesses.
Indeed, Vitamin D receptors (VDR) have been identified in most tissues and cells. It has been observed that many genes may be directly or indirectly regulated by 1,25(OH)2D have provided a rationale for the nonskeletal health benefits of vitamin D.
For example, a study in healthy adults who received either 400 or 2000 IU/d of vitamin D3 for three months in winter reported that 291 genes were either up-regulated or down-regulated. That these genes affected as many as 80 different metabolic pathways (from immune modulation to enhanced antioxidant activity) emphasizes the importance of improving the world’s vitamin D status.
The authors find that the scientific observations that 1,25(OH)2D may also influence epigenetics fully supports the idea that there is no downside to increasing the vitamin D status of adults and children (748).
Thus, it has been shown that Vitamin D deficiency during pregnancy may adversely influence placental development and fetal programming. Also, it is known that Vitamin D deficiency in both parents may influence adverse pregnancy outcomes and susceptibility to developing disease in adult life and even into the next generation.
RECOMMENDATIONS FOR ADEQUATE VITAMIN D3
Drs. Holick and Hossein-nezhad conclude that there is great potential for improving overall health and well-being by increasing serum 25(OH)D levels above 30 ng/mL. They recommend a strategy to prevent vitamin D deficiency and insufficiency. They recommend sensible sun exposure, ingesting foods that contain vitamin D, and taking a vitamin D supplement.
SOURCES OF VITAMIN D3
FOODS IMPORTANT, BUT NOT ALWAYS ENOUGH
Foods can be important sources of vitamin D, but there are few food that naturally contain it. Two good sources are wild-caught salmon and UV-exposed mushrooms, as well as cod liver oil.
Yet, the authors note that an analysis of the vitamin D intake of children and adults in the US revealed that they not able to obtain the RDA for vitamin D from any dietary sources (746). Therefore, if you decide to increase your intake of foods containing vitamin D for the purposes of obtaining adequate vitamin D for health, remember that it can be difficult to obtain sufficient vitamin D from foods alone.
The authors do not dissuade individuals from consuming foods high in vitamin D. However, they suggest that combining dietary sources with sensible sun exposure and vitamin D supplements is the most practical means to attain adequate levels of vitamin D.
SENSIBLE SUN EXPOSURE
While foods (and vitamin D supplements) are essential sources of vitamin D, the most obvious source is sun exposure on skin. Individuals vary in the amount of sunshine they require, typically dependent upon skin tone at the time of expsosure. Individuals with fair skin need less time in the sun to generate adequate levels of vitamin D compared to individuals with darker skin.
The authors assert that an adult in a bathing suit exposed to one minimal erythemal dose (slight pinkness to the skin 24 hours after exposure) is the equivalent to taking approximately 20,000 IU (500 mg) of vitamin D orally (745). By this measure, they find that exposure of arms and legs to 0.5 minimal erythemal dose is equivalent to ingesting approximately 3,000 IU of vitamin D3.
Drs. Holick and Hossein-nezhad suggest that in order to produce adequate vitamin D without burning skin, individuals should expose arms and legs (abdomen and back whenever possible) to sunlight two to three times weekly for approximately 25%–50% of the time it would takes to develop a mild sunburn (i.e., the minimal erythemal dose) (745). Thus, if 30 minutes of midday sun in June will cause a mild sunburn, then just 10–15 minutes of exposure should be enough to produce sufficient vitamin D, according to this measure.
NATURAL SUN PROTECTION
if you plan to remain in the sun after the minimum time required to produce enough vitamin D, then they suggest sun protection. This protection can include wearing proper clothing, including a hat and/or long sleeves, and/or moving yourself into partial shade.
Additional options for sun protection include foods and superfoods. Taking chlorella or Rejuvenate! (original greens) protects skin amazingly well from sun exposure (and speeds healing time for sunburns). Natural astaxanthin is comparably effective to chlorella. I take 10 mg daily (as an extract of the microalga Haematococcus pluvialis), but for maximum protection against sun exposure, take 10–20 mg (i.e., use the higher amount if you are lighter-skinned).
When chlorella and/or astaxanthin is combined with foundational supplements, including a multivitamin, vitamin C and/or antioxidant formulas (like Ultimate Protector), and essential fats, then sun protection is far more complete. Indeed, the body’s antioxidant systems will be supported at optimal levels, and therefore can defend against many different types of free-radical damage, including damage caused by ultraviolet (UV) light.
A diet naturally high in antioxidants therefore powerfully supports the skin’s capacity to protect itself. This is why chlorella and astaxanthin are so effective. Yet, consuming more leafy greens, carrots (and other vegetables with carotenoids), as well as red, purple, and other dark vegetables and fruits is a good idea for helping protect skin health, offers natural sun protection, and provides extra free-radical defense.
AVOID TOXIC COMMERCIAL SUNSCREENS
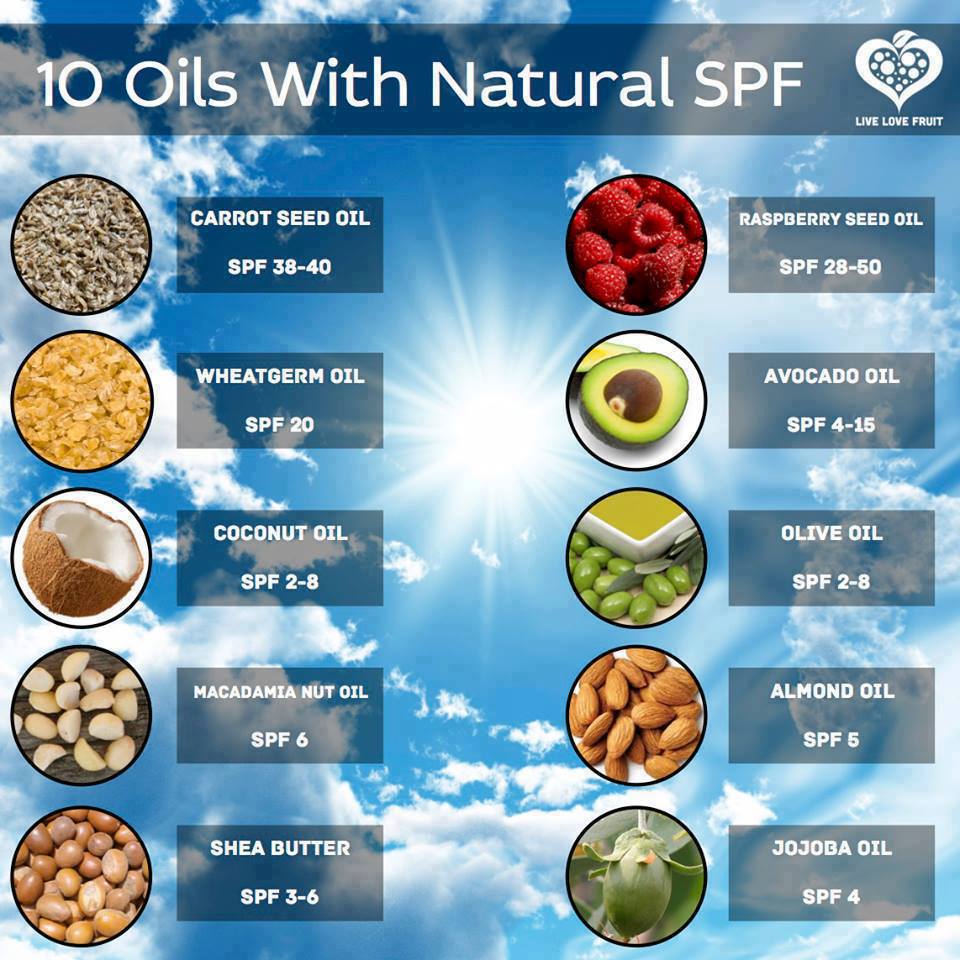
I do not recommend any commercial sunscreens due to the toxic ingredients many contain. However, you might experiment using natural oils with SPF. Carrot oil has an SPF of 38–40. Wheatgerm oil offers an SPF of 20. Even avocado oil has an SPF of 4–15. Coconut and olive oils both offer an SPF of 2–8.
As noted, it is important to consider using natural sunscreens only after the minimum time required to produce adequate vitamin D in the body. In any case, the by-word is “sensible” because staying in the sun beyond the minimum daily time required to produce enough vitamin D is not recommended (unless you protect your skin, e.g., using clothing or natural sun protective substances).
VITAMIN D SUPPLEMENTS
The authors find that vitamin D can be administered daily, weekly, monthly, or every four months to sustain an adequate serum 25(OH)D concentration (746). When taken less often, they recommend significantly higher amounts. They also indicate that for every 100 IU of vitamin D ingested, the blood level of 25(OH)D increases by approximately 0.6 to 1 ng/mL.
I recommend healthy adults take 5,000 IU daily (or several times per week) in the winter. An ideal formula is HPDI’s Vitamin D3 Plus formula, which also provides vitamin A and vitamin K2, which are needed for optimal assimilation and utilization of Vitamin D3.
In the spring and fall, you may be able to reduce your supplemental vitamin D dosage depending on the amount of sun exposure you receive and your dietary intake of vitamin D. In the summer, you may not require any supplemental vitamin D3, if you get sufficient safe sun exposure on a regular basis.
Children require a smaller amount of vitamin D supplementation. The authors recommend 600 IU–1,000 IU per day for kids. This can be accomplished by giving them 1 or 2 small Vitamin D3 Plus softgels weekly.
VITAMIN D SUPPLEMENTS VERY SAFE AT RECOMMENDED LEVELS
Drs. Holick and Hossein-nezhad emphasize the safety of vitamin D even at very high doses, but also remain clear that exceedingly high doses should be avoided. For example, they state that to prevent deficiency in adults, administration of 50,000 IU every two weeks is effective (746).
While 50,000 IU is large single dose, even larger doses of vitamin D (e.g., up to 300,000 IU administered as a bolus) safely have been used initially to reverse extreme deficiency status. Repeated high doses in bolus form have been used in six to twelve month intervals. Nevertheless, they assert that “a steady-state serum 25(OH)D concentration is likely to be maintained by more frequent, lower doses of vitamin D” (746).
GROUPS WITH SPECIAL NEEDS FOR VITAMIN D3
PREGNANT & LACTATING WOMEN REQUIRE MORE VITAMIN D3
Certain groups of individuals require greater amounts of vitamin D. Pregnant and lactating women have higher needs. Human breast milk contains very little vitamin D. Studies show that lactating women must take 4,000–6,000 IU daily to ensure that adequate vitamin D transfers into breast milk to satisfy an infant’s requirements (746).
OBESE INDIVIDUALS
Obese individuals require 2–5 times more vitamin D to treat and prevent vitamin D deficiency because fat can sequester vitamin D (747). This applies to adults and children. Given the dramatic rise in obesity rates in the US and the world, it is little wonder that vitamin D deficiency has become so widespread.
The trend in recent years to avoid sun exposure because of fears of skin damage does not serve the obese population. Sensible sun exposure along with improved diet and use of vitamin D supplements can reverse deficiency among the obese.
While obese persons ideally would focus on losing some weight in order to maximize their long-term health, it is imperative in the immediate term that they obtain sufficient amounts of vitamin D. This would help them avoid deficiency and remain healthy until they are no longer obese, and therefore can gain the benefits of vitamin D without having to obtain significantly higher amounts from diet, sunshine, and/or supplements.
THE ELDERLY
The study authors also point out that the elderly population is at higher risk for clinical complications related to low 25(OH) D levels. With increasing age, the cutaneous production of vitamin D after exposure to solar UV-B radiation decreases due to atrophic skin changes, with a reduced amount of the vitamin D precursor 7-DHC (743).
For example, a comparison of the amount of previtamin D3 produced in skin from individuals aged eight to eighteen with the amounts produced in skin from individuals aged 77–82 reveals that aging can decrease skin’s capacity to produce previtamin D3 by more than two-fold (743). This means that sun exposure ultimately provides less vitamin D for older people.
It would appear that dietary adjustments to include more foods providing vitamin D is important for the elderly. However, vitamin D supplements are probably the most effective means for elderly individuals to maintain adequate levels of vitamin D.
CONCLUSION: VITAMIN D3 SUPPLEMENTS IMPORTANT
In sum, vitamin D supplementation, preferably with vitamin D3 (and supporting nutrients like vitamin K2 and vitamin A), offers an important means for healthy adults and children to obtain sufficient vitamin D year-round. This is particularly the case in winter and in northern latitudes, where no amount of sunshine on skin can generate enough vitamin D to meet daily requirements.
For at risk individuals, including pregnant and lactating women, the obese, and the elderly, vitamin D supplements (as well as foods rich in vitamin D and sensible sun exposure) can help sustain optimal vitamin D levels, and prevent or reverse deficiency.
ADDITIONAL RESOURCES
Article Abstract (mayoclinicproceedings.org)
“Vitamin D for Health: A Global Perspective” (full text .pdf)
HPDI Product Pages
VITAMIN D3 PLUS (HPDI website)
Vitamin D3 Plus Brochure (.pdf 1.3m)
Article Abstracts
Vitamin D Abstracts (HPDI website)
Articles from the HPDI Blog
Vitamin D3 – “SUPERSTAR”!




2 comments
Here is my take, and my own experience…
I would supplement with Vitamin D3 (5,000IUs) at least 5x per week during the winter months and maybe 2x per week during the summer months.
My D levels were still right around 35…
Once I started supplementing with Vitamin K2, the next blood test I took showed my levels were 96! I did NOTHING differently except add the Vitamin K2 to my regiment.
This shows me that the studies I have read that say that those two vitamins need to work together, are true. I believe I am living proof of that.
Hope this helps some. But my Naturopathic doctor says I don’t need vitamin D levels that high, so I am only taking a 5,000IU once a week now.
Rebecca, thanks for sharing your experience! It is interesting that you got such a large benefit from taking Vitamin K2. Can you tell me which form (Mk-4 or Mk-7) and how much (number of micrograms per day) of Vitamin K2 you are taking?
Vitamin K2 is known to be necessary for the proper activation of bone matrix proteins by conferring on them the physical ability to bind calcium (i.e., to build strong bones). In our Vitamin D3 Plus formula we include 10 mcg per softgel of Mk-7.The half-life of Vitamin K2 (as MK-7) is about three days in the body – so will build to about 3 times this much when taken daily.
Chris Masterjohn elegantly discusses the role of Vitamin K2 in bone formation in his groundbreaking article “On the Trail of the Elusive X-Factor: A Sixty-Two-Year-Old Mystery Finally Solved” (see Weston A. Price Foundation website). Because Vitamin K2 is needed to facilitate the function of Vitamin D in proper bone formation (including tooth structure), Masterjohn states that Vitamin D toxicity is most likely a case of Vitamin K2 deficiency. It is clear that adequate Vitamin K2 both protects against Vitamin D toxicity and supports the effective use of Vitamin D in the body.
I have seen no research that indicates blood levels of Vitamin D3 will increase dramatically when Vitamin K2 is taken. If others can repeat your experience with Vitamin K2, important knowledge will have been gained!